Thioprine

Thioprine
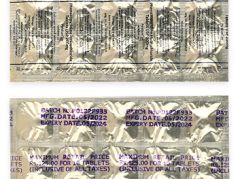
- In our pharmacy, you can buy thioprine without a prescription, with delivery in 5–14 days throughout Australia. Discreet and anonymous packaging.
- Thioprine (azathioprine) is prescribed for autoimmune conditions such as rheumatoid arthritis, inflammatory bowel disease (IBD), and lupus, as well as for preventing organ transplant rejection. It acts as an immunosuppressant by inhibiting the synthesis of purines, which are necessary for the proliferation of immune cells.
- The usual dosage of thioprine varies: for autoimmune disorders, it is typically 1–3 mg/kg/day, while for transplant patients, it ranges from 3–5 mg/kg/day.
- The form of administration is oral tablets or injectable forms for hospital use.
- The effect of the medication begins within 6–12 weeks for autoimmune diseases.
- The duration of action can vary but is generally sustained with continuous use.
- Do not consume alcohol.
- The most common side effect is gastrointestinal issues like nausea and vomiting.
- Would you like to try thioprine without a prescription?
Basic Thioprine Information
- International Nonproprietary Name (INN): Azathioprine
- Brand names available in Australia: Imuran
- ATC Code: L04AX01
- Forms & dosages: Tablets (25 mg, 50 mg, 75 mg, 100 mg)
- Manufacturers in Australia: Aspen Pharma, various approved generics
- Registration status in Australia: Prescription (Rx) only
- OTC / Rx classification: Prescription only (Rx)
Everyday Use & Best Practices
Establishing a routine for taking thioprine is crucial to maximise its effectiveness, particularly for those in Australia who juggle busy daily schedules. A consistent dosing time, whether in the morning or evening, helps maintain stable drug levels in the body. This can be tailored to fit individual lifestyles, allowing patients to create a manageable habit without disruption.
For morning users, integrating thioprine into daily rituals such as breakfast can aid memory. Evening dosing might work better for those who prefer taking medications before bed, ensuring a peaceful night without prompting multiple reminders throughout the day.
Taking With or Without Meals
The timing of thioprine intake concerning meals can influence its absorption. Patients are generally advised to adhere to the following recommendations:
- Taking thioprine with food can help minimise gastrointestinal side effects.
- However, it's essential to note that some high-fat meals might inhibit absorption, leading to decreased effectiveness.
To optimise the benefits, it's often best to find a consistent pattern – whether taking thioprine an hour before eating or two hours after. Staying within these guidelines can significantly enhance drug absorption.
Safety Priorities
While thioprine can be an effective treatment option for many, certain groups should avoid this medication, as per the Therapeutic Goods Administration (TGA) guidelines. Key contraindications include:
- Individuals with known hypersensitivity to azathioprine.
- People facing active infections, as immunosuppression can worsen their condition.
- Patients with severe liver disease need to be careful due to heightened risk of toxicity.
- Pregnant individuals should generally refrain from thioprine due to potential teratogenic effects.
Activities To Limit
Amidst treatment with thioprine, patients should be aware of certain activities that may necessitate caution. Both driving and operating heavy machinery can pose risks due to potential side effects like dizziness or fatigue. Additionally, workplace safety may take precedence, where tasks requiring high concentration may need adjustment while adapting to the medication. Regular monitoring of side effects, especially during the initial treatment phase, is advisable.
Dosage & Adjustments
According to Pharmaceutical Benefits Scheme (PBS) guidelines, the starting dose of thioprine typically ranges based on the condition being treated and patient weight. For most indications, a common regimen might be:
- Initial dosages fall between 1 to 3 mg/kg/day, divided into once or twice daily doses.
- For transplant patients, dosages usually start higher, ranging from 3 to 5 mg/kg/day, adjusted based on clinical response and side effects.
It's important to note that special populations, such as the elderly or those with comorbidities, may require tailored adjustments. For instance, older adults might need lower initial dosages, given their increased risk of complications from myelosuppression. Similarly, adjustments may be required for Indigenous health; individual characteristics should inform any alterations in dosing.
User Testimonials
A review of Australian patient feedback on thioprine reveals a generally positive outlook. Many patients highlight improved quality of life and disease management through forums and testimonials. Notably, individuals living with autoimmune diseases often express satisfaction with their treatment plans, reporting enhanced energy levels and fewer flare-ups as a result of consistent thioprine use.
On the other hand, community discussions also unearth common challenges associated with thioprine usage. Side effects like nausea and a temporary dip in white blood cell counts are frequently cited issues. Managing medication alongside these experiences, while seeking support through forums can be crucial in navigating the journey of treatment while feeling supported within the community.
Buying Guide
When considering where to purchase thioprine in Australia, several reputable pharmacy chains offer easy access to the medication. Notably:
- Chemist Warehouse – Known for competitive pricing and accessibility.
- Priceline – Often offers various brands and forms of thioprine.
- TerryWhite Chemmart – Provides professional pharmacy services alongside medication.
Price Considerations: Depending on your prescription status, costs can vary significantly. For those eligible for the PBS, medication costs will typically be lower than private purchases, making it economically viable to explore subsidised options. Patients are encouraged to inquire about pricing at different pharmacies to find competitive rates.
What’s Inside & How It Works
When considering the use of thioprine, understanding its foundational elements is crucial. The active ingredient in thioprine, known as azathioprine, plays a vital role in regulating the immune system. It’s an immunosuppressant, meaning it limits the body's defensive responses, which can be beneficial for individuals with autoimmune conditions or those who have undergone organ transplants.
Ingredients Overview
Azathioprine, the primary ingredient in thioprine, is recognised for its effectiveness in various treatments. Acting as a purine analogue, it interferes with DNA synthesis. This disruption is particularly useful in conditions where the immune system attacks the body's own tissues, such as in rheumatoid arthritis or lupus.
Mechanism Basics Explained Simply
The way thioprine works in the body is quite straightforward. Once ingested, azathioprine gets converted into active forms that inhibit the proliferation of lymphocytes, a type of white blood cell involved in immune responses. By reducing the number of these cells, thioprine decreases inflammation and tissue damage. For patients, this means a potential reduction in the severity of symptoms and a lower chance of complications from autoimmune disorders. However, it's paramount that patients remain under regular medical supervision as the immunosuppressive effects also heighten the risk of infections and other health issues.
Main Indications
For those contemplating thioprine usage, knowing its approved applications is essential. The Therapeutic Goods Administration (TGA) in Australia has listed thioprine for several key conditions, underscoring its importance in therapeutic contexts.
Approved Uses Under TGA
- Rheumatoid arthritis
- Inflammatory bowel disease (IBD)
- Lupus erythematosus
- Kidney transplantation
These conditions highlight thioprine’s role in managing chronic diseases where immune modulation can significantly improve patient quality of life.
Off-Label Uses in Australian Clinics
Beyond its approved uses, thioprine is frequently employed off-label in clinical settings, marking its versatility. Common applications include treatment for other autoimmune disorders and certain skin conditions, such as dermatitis or vasculitis. Clinical experience supports its efficacy in these cases, and numerous studies have sought to evaluate its benefits further, confirming the potential advantages of thioprine in broader medical contexts.
Interaction Warnings
Understanding interactions with food and medications is crucial for safe thioprine use. Certain dietary elements can impact how thioprine works and should be approached with caution.
Food Interactions
Patients using thioprine are advised to be mindful of dietary habits. Here are a few considerations:
- Alcohol: Consumption can aggravate liver effects, increasing toxicity risks.
- Caffeine: Interaction is minimal, but excess intake might lead to increased side effects.
- General Diet: A balanced diet supports immune health, which is vital during thioprine treatment.
Drug Conflicts Tracked by TGA & PBS
The TGA and Pharmaceutical Benefits Scheme (PBS) consistently monitor potential drug interactions with thioprine. Notable interactions include:
- Allopurinol: Increases azathioprine toxicity.
- Other immunosuppressants: Heightened risk of serious side effects.
For the best outcomes, patients should communicate openly with their healthcare providers about all medications and supplements being taken.
Latest Evidence & Insights
Research surrounding thioprine continues to evolve, with significant contributions from both Australian and international studies between 2022 and 2025, focusing on efficacy and safety.
Recent findings underscore thioprine's effectiveness across various conditions:
- Notable reports have highlighted increased patient survival rates in transplant scenarios.
- Safety studies indicate manageable side effects with appropriate monitoring.
- Emerging insights suggest genetic factors might influence treatment outcomes, paving the way for personalised medicine.
As research progresses, recognising the balance between benefits and risks will remain paramount for patients using thioprine.
Alternative Choices
When comparing alternatives to thioprine, various immunosuppressants come to light. Each has its own set of pros and cons that could influence a patient's choice. Below is a comparative table highlighting some commonly used options:
| Immunosuppressant | Pros | Cons |
|---|---|---|
| Mycophenolate mofetil | Effective in organ transplant and autoimmune diseases. Less risk of myelosuppression. | Gastrointestinal side effects. Requires consistent dosage adherence. |
| Methotrexate | Well-established for rheumatoid arthritis. Can improve patient quality of life. | Potential for liver toxicity. Requires regular monitoring. |
| Tacrolimus | Highly effective in transplant settings. Quick action with targeted effects. | Risk of nephrotoxicity and infections. Requires careful dosing. |
| Cyclosporine | Long clinical use in transplants. Reduces rejection rates significantly. | Can cause hypertension and kidney impairment. Daily monitoring essential. |
| Mercaptopurine | Similar mechanism to thioprine. Useful in certain types of leukaemia. | Increased risk of myelosuppression. Clinical use limited compared to thioprine. |
Regulation Snapshot
The Therapeutic Goods Administration (TGA) in Australia plays a critical role in approving medications such as thioprine and determining their safety and efficacy for public use.
The TGA approval process involves rigorous evaluation through clinical trials to ensure that drugs meet strict regulatory standards. This ensures that patients receive medications that are both safe and effective.
Once approved, the Pharmaceutical Benefits Scheme (PBS) assesses whether a drug can be subsidised for public use. PBS subsidy enables easier access for patients as it significantly reduces out-of-pocket costs for numerous essential medications.
These regulatory frameworks are essential in enhancing patient access to effective therapies while adhering to high safety standards. It encourages adherence to treatment regimens and fosters trust in the healthcare system.
FAQ Section
Some common questions patients often ask during pharmacy consultations regarding thioprine include:
- What should I do if I miss a dose of thioprine?
It's advised to take the missed dose as soon as you remember if it’s within 12 hours. If it’s closer to your next scheduled dose, skip the missed one. Never double up to make up for a missed dose. - Are there any side effects I should be aware of?
Yes, common side effects include nausea, fatigue, and potential liver enzyme elevation. Report any unusual symptoms to a healthcare professional immediately. - How long will I need to take thioprine?
Duration varies. For autoimmune diseases, it might be a long-term management strategy, while in transplant cases, it could be lifelong with periodic adjustments. - Can thioprine affect my fertility?
There are considerations and potential risks, so discuss with a healthcare provider if planning for pregnancy or if fertility is a concern.
Guidelines for Proper Use
For pharmacists counselling patients about thioprine, consider the following guidelines:
- Monitor blood counts: Regular monitoring is crucial, especially during the initial treatment phase, to check for any adverse hematologic effects.
- Educate on side effects: Inform patients about possible side effects and when to seek medical advice. Emphasise the importance of adherence to prescribed doses.
- Discuss interactions: Patients should be made aware of potential interactions with other medications and the need to disclose all current treatments.
- Provide storage guidelines: Stress the importance of storing thioprine at 20–25°C, keeping it protected from light and moisture.
- Encourage open communication: Encourage patients to discuss any concerns or questions regarding their treatment, fostering a trusting pharmacist-patient relationship.